A pain medication taken by millions of people worldwide may pose far greater health risks than previously believed, according to a major new analysis that raises concerns about its safety—particularly for older adults and those with underlying heart disease.
Researchers have found that tramadol, one of the most commonly prescribed opioid painkillers globally, delivers minimal benefit for chronic pain relief while significantly increasing the risk of serious adverse health events, including potentially deadly cardiovascular complications.
The findings come from a large Danish review of clinical trial data that challenges decades-long assumptions about tramadol’s effectiveness and safety profile. The drug has been prescribed for nearly 50 years and is often favored by physicians because it is perceived as less addictive and less dangerous than stronger opioids such as oxycodone or fentanyl.
However, the new analysis suggests that this perception may be dangerously misleading.
Minimal Pain Relief, Major Health Risks
The researchers examined data from 19 randomized clinical trials involving more than 6,500 patients who were treated with either tramadol or a placebo for various forms of chronic pain. The average participant was 58 years old—an age group already at elevated risk for cardiovascular disease.
Across the studies, tramadol provided only a slight reduction in pain compared to placebo, an effect the researchers described as clinically insignificant. At the same time, patients taking the drug were more than twice as likely to experience a serious adverse event.
Compared with placebo, tramadol users had a 113 percent higher likelihood of suffering a serious medical complication of any kind, the analysis found.
“These results suggest that tramadol may offer little meaningful benefit for chronic pain while substantially increasing the risk of harm,” the researchers concluded.
Cardiac Events a Key Driver of Risk
While the analysis looked broadly at all serious adverse events, researchers found that the elevated risk was largely driven by an increase in cardiac complications and cancer-related conditions.
Reported heart-related events included chest pain, coronary artery disease (CAD), heart attacks, and congestive heart failure. Although the study did not quantify the precise risk increase for each specific condition, the overall pattern raised red flags for clinicians.
Coronary artery disease affects more than 18 million Americans and is the leading cause of heart attacks, heart failure, and cardiovascular death. Many individuals with CAD remain undiagnosed until a major event occurs, making drug-related triggers especially dangerous.
The researchers noted that tramadol is frequently prescribed to older adults for chronic conditions such as arthritis and back pain—precisely the population most vulnerable to cardiovascular disease.
A Common Prescription With Broad Reach
Tramadol is among the most widely prescribed opioid medications in the United States, with more than 16 million prescriptions filled in 2023 alone. In many countries, it is often one of the first opioid options offered for moderate to severe pain because of its Schedule IV classification by the U.S. Drug Enforcement Administration, indicating a lower perceived risk of abuse and dependence.
Despite that classification, tramadol still acts on opioid receptors in the brain and carries addiction potential, as well as a range of known side effects including nausea, dizziness, constipation, and sedation.
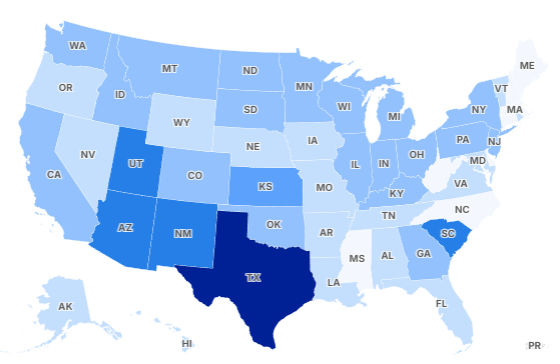
The Danish researchers emphasized that no precise national data exist tracking tramadol use specifically among heart disease patients. However, demographic overlap strongly suggests that many people with cardiovascular risk factors are routinely exposed to the drug.
Why the Findings Matter Now
The results arrive at a time when physicians are under intense pressure to balance pain management with safety amid an ongoing opioid crisis. Doctors are urged to reduce opioid prescribing, yet are still responsible for addressing legitimate, often debilitating pain.
Tramadol has long been viewed as a compromise solution—a “safer” opioid that could ease suffering without the dangers associated with stronger narcotics. The new findings call that assumption into question.
“The potential harms associated with tramadol use for pain management likely outweigh its limited benefits,” the researchers wrote, urging clinicians to reconsider routine prescribing of the drug.
While the study stops short of calling for regulatory agencies to withdraw tramadol from the market, it strongly recommends that healthcare providers explore safer alternatives whenever possible.
Alternatives to Opioid-Based Pain Management
The authors suggest that non-opioid medications and non-pharmacological therapies should be prioritized for chronic pain treatment, particularly in older adults or patients with cardiovascular risk.
Such approaches may include acetaminophen or nonsteroidal anti-inflammatory drugs (when appropriate), targeted physical therapy, structured exercise programs, and cognitive behavioral therapy. In some cases, multidisciplinary pain management strategies have been shown to reduce reliance on medications altogether.
Experts caution that no pain treatment is entirely risk-free, but emphasize that therapies should be chosen based on a careful assessment of both benefit and harm.
Implications for Patients
Health professionals stress that patients currently taking tramadol should not stop the medication abruptly without consulting their doctor, as sudden discontinuation can lead to withdrawal symptoms.
Instead, patients—particularly those with heart disease, high blood pressure, or a family history of cardiovascular problems—are encouraged to discuss the findings with their healthcare providers and evaluate whether alternative treatments may be safer.
The study was published in The BMJ, one of the world’s leading medical journals, adding significant weight to its conclusions.
A Shift in Perspective
For decades, tramadol has occupied a unique position in pain medicine: widely used, generally trusted, and considered relatively low risk. This new analysis suggests that reputation may no longer be justified.
As evidence continues to accumulate, experts say the medical community may need to rethink how pain is treated—moving away from default opioid use and toward approaches that prioritize long-term safety as much as symptom relief.
James Jenkins is a celebrated Pulitzer Prize-winning author whose work has reshaped the way readers think about social justice and human rights in America. Raised in Atlanta, Georgia, James grew up in a community that instilled in him both resilience and a strong sense of responsibility toward others. After studying political science and creative writing at Howard University, he worked as a journalist covering civil rights issues before dedicating himself fully to fiction. His novels are known for their sharp, empathetic portraits of marginalized communities and for weaving personal stories with broader political realities. Jenkins’s breakout novel, Shadows of Freedom, won national acclaim for its unflinching look at systemic inequality, while his more recent works explore themes of identity, resilience, and the fight for dignity in the face of oppression. Beyond his novels, James is an active public speaker, lecturing at universities and participating in nonprofit initiatives that support literacy and community empowerment. He believes that storytelling is a way to preserve history and inspire change. When not writing, James enjoys jazz music, mentoring young writers, and traveling with his family to explore cultures and stories around the world.