The debate over COVID-19 policies—ranging from lockdowns to school closures to vaccine mandates—has reignited with the release of a new peer-reviewed study that is prompting experts to rethink some of the most widely held beliefs about the pandemic’s global response.
Over the past few years, narratives surrounding vaccine efficacy, government mandates, and the overall cost-benefit of sweeping health interventions have sharply divided both public opinion and the scientific community. While some argue that swift action saved millions of lives, others claim those very efforts sowed distrust and caused collateral damage to mental health, education, and economic stability. Until now, many global agencies and institutions operated on models that assumed large-scale immunization campaigns were responsible for saving tens of millions of lives. That assumption has been critical in justifying various policy choices during the pandemic.
However, a recent analysis is now calling those earlier figures into question. Rather than providing finality to the ongoing debate, the findings introduce a layer of complexity and nuance—particularly regarding who benefited most from vaccination and whether the aggressive push for universal inoculation might have come at the cost of reduced public trust.
Midway through the study’s conclusions, one detail has emerged as particularly striking: the new estimate suggests that approximately 2.5 million lives were saved by COVID-19 vaccines from 2020 to 2024—far fewer than the roughly 20 million lives some models projected were saved in just the first year of rollout.
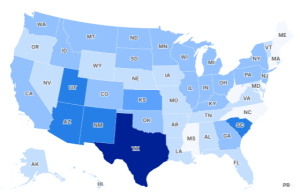
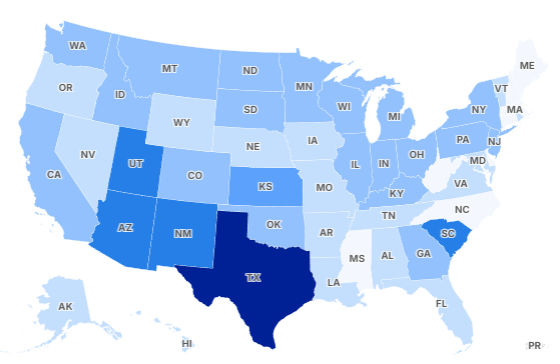
Published in JAMA Health Forum, the study was conducted by three researchers, including epidemiologist Dr. John P. A. Ioannidis of Stanford University. The data reveals that 90% of the lives saved were individuals over the age of 60, with an overwhelming majority of those vaccines being administered before infection. The paper estimates that one death was prevented for every 5,400 vaccine doses given globally during that four-year period. Additionally, for every 900 doses, one year of human life was saved—adding up to approximately 14.8 million life-years overall.
Among younger age groups, particularly those under 30, the life-saving impact of the vaccines was minimal. Out of roughly 4 billion people in that age bracket, the study estimates that just 2,000 lives were saved by vaccination. For those aged 30 to 59—nearly 3 billion people worldwide—vaccines were estimated to have prevented approximately 250,000 deaths.
This data has renewed calls from medical experts to reconsider one-size-fits-all vaccination strategies for future pandemics. One such expert is Dr. Monica Gandhi, a University of California–San Francisco medical professor and epidemiologist, who supported the study’s conclusion that future vaccine rollouts should prioritize older and more vulnerable populations. She further pointed out that the closure of schools in the U.S. during the pandemic caused significant harm—particularly learning loss among children from low-income backgrounds—and was not necessary to protect children.
Dr. Ioannidis also criticized the messaging and tactics used to promote COVID-19 vaccination, especially among the young and healthy. He argued that mandates and coercive language may have had unintended consequences, such as discouraging those at higher risk—older adults and people with serious medical conditions—from seeking vaccination. “The mandates and the aggressive push to vaccinate everyone probably did not help,” he said. “The coercive, almost messianic messaging caused damage to public health with an increase in vaccine hesitancy and loss of trust in medicine and medical science.”
Importantly, the study does not align itself with vaccine skepticism. On the contrary, Ioannidis noted that while previous estimates may have been overly optimistic, the study also refutes “exaggerated estimates” from vaccine critics who claim the shots killed millions. “We are open to revising our estimates if better data arise in the future,” he stated.
As for the political implications, familiar figures have already begun to weigh in. While not directly related to the study, the long-standing feud between Senator Rand Paul and former White House medical advisor Dr. Anthony Fauci re-entered the spotlight after the senator referred Fauci to the Justice Department, citing alleged contradictions in his previous testimonies about pandemic policies.
Ultimately, the study’s authors advocate for more data transparency, better long-term studies, and future pandemic responses that rely more heavily on risk stratification and less on blanket strategies. The full text is available through JAMA Health Forum and is already fueling intense discussion in public health circles and policymaking spheres alike.

Emily Johnson is a critically acclaimed essayist and novelist known for her thought-provoking works centered on feminism, women’s rights, and modern relationships. Born and raised in Portland, Oregon, Emily grew up with a deep love of books, often spending her afternoons at her local library. She went on to study literature and gender studies at UCLA, where she became deeply involved in activism and began publishing essays in campus journals. Her debut essay collection, Voices Unbound, struck a chord with readers nationwide for its fearless exploration of gender dynamics, identity, and the challenges faced by women in contemporary society. Emily later transitioned into fiction, writing novels that balance compelling storytelling with social commentary. Her protagonists are often strong, multidimensional women navigating love, ambition, and the struggles of everyday life, making her a favorite among readers who crave authentic, relatable narratives. Critics praise her ability to merge personal intimacy with universal themes. Off the page, Emily is an advocate for women in publishing, leading workshops that encourage young female writers to embrace their voices. She lives in Seattle with her partner and two rescue cats, where she continues to write, teach, and inspire a new generation of storytellers.