More than 30,000 prescription cholesterol medications have been recalled across the United States after federal regulators identified potency and dissolution problems that could affect how well the drugs work in patients, according to recent recall notices issued by the Food and Drug Administration.
The recalls involve two widely prescribed cholesterol-related medications manufactured and distributed by separate pharmaceutical companies. While the FDA has classified both actions as Class II recalls—meaning the products are unlikely to cause serious or permanent harm—officials warn that the affected drugs may lead to inconsistent therapeutic effects and potential side effects if taken as prescribed.
Thousands of Bottles of Omega-3 Drug Recalled
The larger of the two recalls involves nearly 23,000 bottles of icosapent ethyl capsules, a prescription omega-3 fatty acid medication commonly used to lower high triglyceride levels and reduce the risk of cardiovascular disease.
New Jersey-based Zydus Pharmaceuticals voluntarily recalled 22,896 bottles of the drug, which were packaged in 120-count bottles containing 1-gram capsules. The FDA classified the recall as a Class II action on January 22.
According to the agency, the recall was initiated due to sub-potency issues discovered during quality testing. Specifically, the FDA said the problem stemmed from oxidation caused by leakage of the capsule contents, which may result in reduced effectiveness of the medication.
“Due to oxidation caused by leakage of the contents, use of the affected product may lead to inconsistent therapeutic effects and an increase in potential gastrointestinal side effects in some patients,” the FDA stated in its recall notice.
The medication was manufactured by Softgel Healthcare Pvt. Ltd., an India-based pharmaceutical manufacturer, and distributed throughout the United States by Zydus Pharmaceuticals. The recalled product was intended for prescription use only.
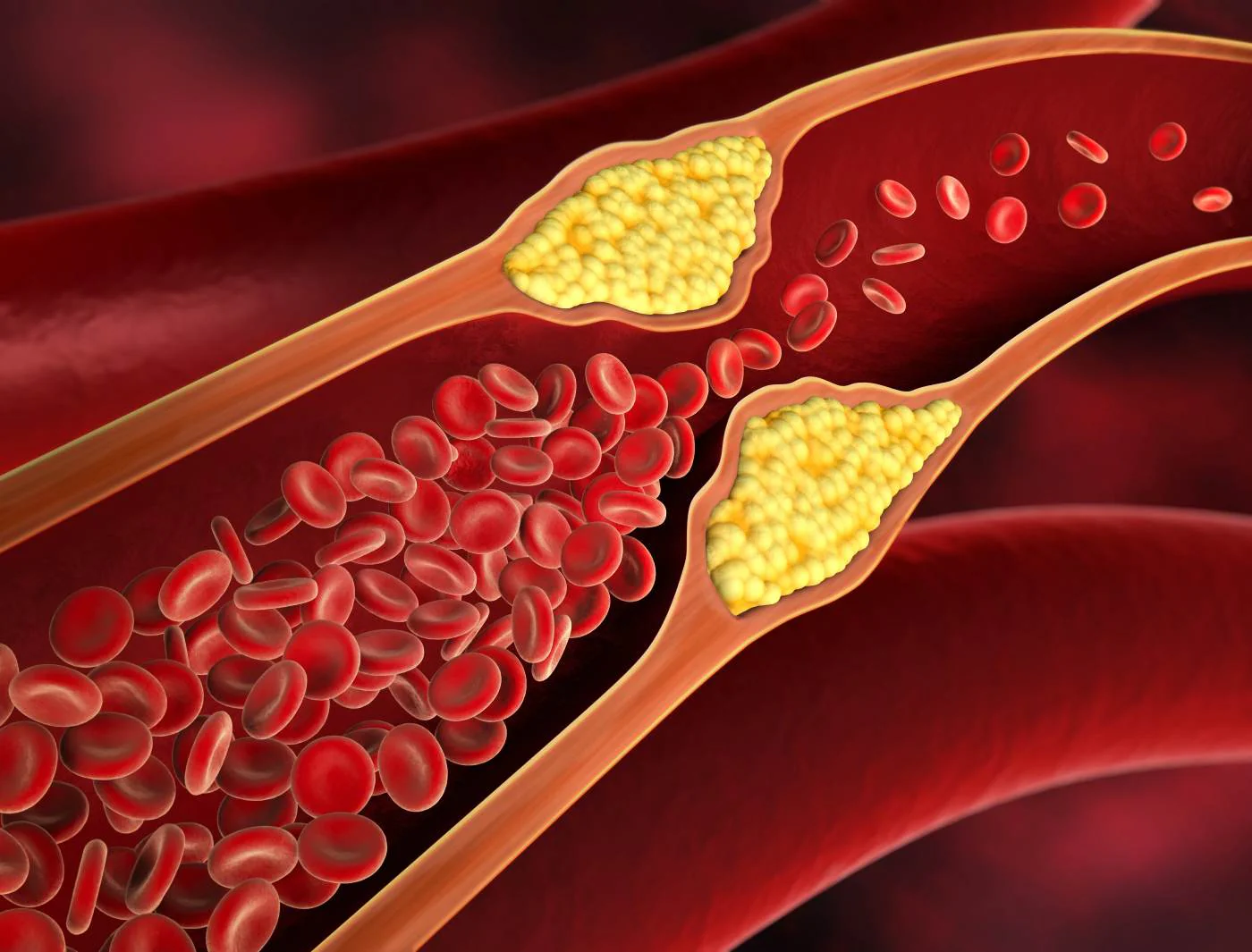
Icosapent ethyl is often prescribed to patients with elevated triglyceride levels who are already taking statin medications but require additional lipid control. It is also commonly recommended for patients at increased risk of heart attack or stroke.
While the FDA has not reported any serious injuries linked to the recalled batches, patients taking the affected product may not receive the full cardiovascular protection intended by the medication.
Statin Drug Also Pulled From Market
In a separate recall issued days earlier, pharmaceutical distributor AvKare announced the recall of 7,991 cartons of rosuvastatin tablets, another widely prescribed cholesterol medication.
The recalled rosuvastatin products were packaged in 50-tablet cartons containing 10-milligram doses. The FDA classified this recall as a Class II action on January 20.
According to the agency, the drug failed to meet established dissolution specifications during routine quality testing. Dissolution testing measures how quickly and effectively a tablet breaks down in the body—a critical factor in determining whether the medication is absorbed properly into the bloodstream.
When a drug does not dissolve as expected, it may not deliver the intended dose to the patient, potentially reducing its effectiveness in controlling cholesterol levels.
Rosuvastatin, commonly marketed under the brand name Crestor, is a statin medication used to lower LDL (“bad”) cholesterol and triglycerides while increasing HDL (“good”) cholesterol. It is one of the most frequently prescribed cholesterol drugs in the United States, with tens of millions of prescriptions filled annually.
Because statins are often taken long-term to manage chronic cardiovascular risk, even minor deviations in drug quality can have meaningful effects over time, particularly for patients with existing heart disease or diabetes.
What a Class II Recall Means for Patients
The FDA defines a Class II recall as a situation in which use of the affected product may cause temporary or medically reversible adverse health consequences, or where the likelihood of serious harm is considered remote.
In both cases, the agency emphasized that patients should not stop taking their prescribed medication abruptly without consulting their healthcare provider. Sudden discontinuation of cholesterol-lowering drugs can increase the risk of heart attack or stroke, particularly in high-risk individuals.
Patients who believe they may have received a recalled product are encouraged to check the lot numbers on their prescription bottles and contact their pharmacist or prescribing physician for guidance. In most cases, pharmacies can provide replacement medication from unaffected batches.
Part of a Broader Pattern of Drug Quality Recalls
The recent recalls come amid a growing number of FDA enforcement actions involving cardiovascular medications over the past year.
Several months earlier, at least 140,000 bottles of generic atorvastatin—a commonly prescribed cholesterol drug—were recalled nationwide after failing dissolution specifications. That recall affected multiple manufacturers and dosage strengths.
Last August, the FDA also recalled tens of thousands of bottles of blood pressure and heart medications due to contamination with nitrosamines, a class of chemical compounds linked to increased cancer risk. Those recalls included more than 88,000 bottles of carvedilol tablets and 20,000 bottles of metoprolol tartrate tablets, both widely used to treat hypertension and heart failure.
Regulators have increased scrutiny of pharmaceutical manufacturing processes in recent years, particularly for drugs produced overseas and distributed in the U.S. supply chain. While most recalled products do not result in serious injury, the frequency of such actions has raised concerns about quality control and oversight in the global drug manufacturing system.
FDA Emphasizes Monitoring and Reporting
The FDA continues to encourage patients and healthcare providers to report adverse events or quality concerns through its MedWatch reporting system. Such reports often play a key role in triggering investigations and recalls.
In statements accompanying recent recall notices, the agency reiterated that it routinely conducts inspections, reviews quality testing data, and works with manufacturers to identify and correct deficiencies before they result in patient harm.
For now, officials stress that the recalls are precautionary and that the overall benefit of cholesterol-lowering medications remains well established.
Still, the latest actions serve as a reminder that even widely used prescription drugs are subject to manufacturing errors—and that patients should stay informed, check their prescriptions, and communicate promptly with healthcare providers when recalls are announced.

Emily Johnson is a critically acclaimed essayist and novelist known for her thought-provoking works centered on feminism, women’s rights, and modern relationships. Born and raised in Portland, Oregon, Emily grew up with a deep love of books, often spending her afternoons at her local library. She went on to study literature and gender studies at UCLA, where she became deeply involved in activism and began publishing essays in campus journals. Her debut essay collection, Voices Unbound, struck a chord with readers nationwide for its fearless exploration of gender dynamics, identity, and the challenges faced by women in contemporary society. Emily later transitioned into fiction, writing novels that balance compelling storytelling with social commentary. Her protagonists are often strong, multidimensional women navigating love, ambition, and the struggles of everyday life, making her a favorite among readers who crave authentic, relatable narratives. Critics praise her ability to merge personal intimacy with universal themes. Off the page, Emily is an advocate for women in publishing, leading workshops that encourage young female writers to embrace their voices. She lives in Seattle with her partner and two rescue cats, where she continues to write, teach, and inspire a new generation of storytellers.